Nanobots could be the next big breakthrough in cancer treatment by precisely targeting tumors and releasing deadly agents, all while sparing healthy tissue. They use innovative mechanisms like environment-responsive activation, magnetic guidance, and DNA origami structures. Recent animal studies show remarkable tumor shrinkage and even complete disappearance in some cases. Challenges remain for human trials, but ongoing advancements suggest nanobots could revolutionize surgery and therapy—keep exploring to discover how this technology might reshape cancer care.
Key Takeaways
- Nanobots can precisely target and deliver therapies directly to cancer cells, minimizing damage to healthy tissue.
- They respond to tumor-specific cues like acidity and surface markers for highly selective attack.
- Recent studies show nanobots effectively shrink tumors and can completely eradicate some, demonstrating promising therapeutic results.
- Combining nanobots with gene editing, immune activation, and existing treatments enhances overall cancer therapy effectiveness.
- Challenges remain in clinical translation, including safety regulation, accurate human models, and long-term monitoring for widespread use.
How Nanorobots Target Tumors With Precision
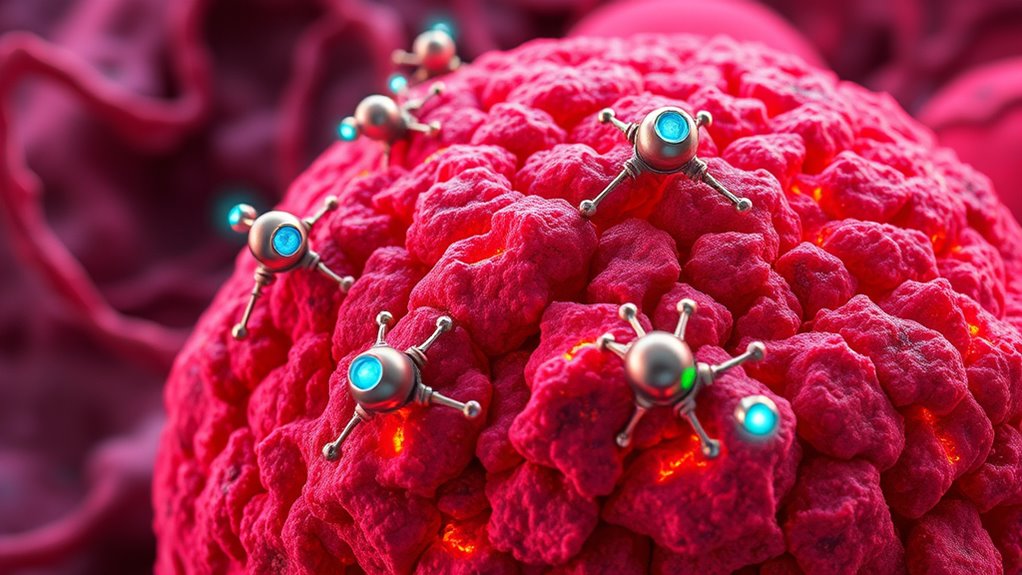
Nanorobots achieve precise tumor targeting by leveraging tumor-specific markers and environmental cues. You can think of them as smart delivery vehicles that recognize unique proteins or peptides on tumor cells, like nucleolin or other biomarkers. These nanobots bind selectively to the tumor’s surface, avoiding healthy tissue. They also respond to environmental signals such as acidity, which is common in tumor microenvironments. When they reach the tumor, they activate their payloads—like peptides, drugs, or enzymes—only under these specific conditions. This guarantees they deliver treatment directly where needed, reducing side effects. Magnetic guidance and sensors help steer nanobots toward the tumor, enhancing accuracy. By combining surface recognition with environmental triggers, nanorobots provide a highly precise approach to targeting cancer cells. Incorporating essential oils for targeted therapy strategies could potentially improve nanobot efficiency and minimize side effects further. Additionally, advancements in nanobot design are exploring ways to improve their stability and responsiveness within the complex tumor environment. Moreover, ongoing research into reconditioning batteries can inspire innovative energy solutions for powering nanorobots, ensuring they operate efficiently within the body. Furthermore, innovations in biocompatible materials are crucial for ensuring safe and effective operation inside the human body, especially considering the challenges of biological compatibility and immune response.
Innovative Mechanisms Powering Cancer-Fighting Nanodevices

Innovative mechanisms enable cancer-fighting nanodevices to target tumors with remarkable precision and effectiveness. Many nanobots are designed to activate only in the tumor’s acidic microenvironment, sparing healthy tissue. Magnetic propulsion guides nanodevices directly to cancer sites, then sensors detect oxygen gradients for accurate localization. DNA origami structures unfold within tumors to expose lethal peptides, destroying cancer cells from inside. Some nanobots deliver enzymes that break down their shells, releasing drugs directly where needed. Others coagulate blood vessels using thrombin, starving tumors of oxygen. Nanoparticles can also enhance radiotherapy by increasing tumor sensitivity. These mechanisms work together, allowing nanobots to act selectively and efficiently, pushing the boundaries of targeted cancer treatment and minimizing side effects. Additionally, the development of these nanodevices is supported by ongoing research into Youngster Choice and natural biological processes, which helps improve their design and effectiveness. Advances in biocompatibility are crucial for ensuring that nanodevices operate safely within the human body without provoking adverse immune responses.
Breakthrough Animal Study Results in Tumor Reduction

Recent animal studies have demonstrated remarkable tumor reductions using nanobots, highlighting their potential as effective cancer treatments. You can imagine these tiny devices actively seeking out cancer cells, delivering targeted therapies, and shrinking tumors. For example:
Animal studies show nanobots dramatically shrink tumors, offering new hope for targeted cancer treatments.
- Visualize nanobots binding to tumor blood vessels, releasing peptides that cut off oxygen supply.
- Picture DNA origami nanorobots unfolding within the tumor environment, releasing lethal agents precisely where needed.
- Envision nanobots guiding chemotherapy, increasing its potency by 20,000 times and halting leukemia progression.
- Understanding the self‑defense mechanisms of cancer cells can help improve nanobot targeting and avoid resistance, making treatments more effective and sustainable. Additionally, ongoing research into targeted delivery systems aims to enhance the precision of nanobot therapies. In mice, researchers achieved up to 90% tumor size reduction, with some tumors disappearing completely. These results showcase how nanobots can selectively target and destroy cancer cells while sparing healthy tissue, demonstrating their groundbreaking potential in cancer therapy. Moreover, advancements in biocompatible materials are crucial for ensuring the safety and stability of nanobots inside the body. Incorporating advanced imaging techniques can also improve the tracking and control of nanobots during treatment, further increasing their efficacy.
Overcoming Challenges for Human Clinical Trials

To move nanobots into human trials, you’ll need to navigate complex regulatory approvals that ensure safety and efficacy. Developing accurate animal models that closely mimic human disease is essential for predicting how these nanobots will perform in people. Addressing these challenges head-on will be vital for translating promising results into real-world cancer treatments. Incorporating Indigenous wellness practices into research protocols may also provide innovative perspectives on holistic health approaches that could enhance patient outcomes. Recognizing the importance of clinical trial design can further improve the success rate of new therapies entering the market. Additionally, establishing reliable preclinical testing methods is critical for assessing nanobots’ safety before human trials. Ensuring robust quality control throughout the development process can prevent potential setbacks and build trust with regulatory bodies. Implementing standardized testing protocols can further streamline approval processes and ensure consistent safety standards.
Regulatory Approvals Needed
Advancing nanobot therapies from laboratory success to human clinical trials requires traversing a complex regulatory landscape. You need to demonstrate safety, efficacy, and manufacturing consistency to gain approval. Here are the key steps:
- Rigorous safety testing: You must show nanobots won’t harm healthy tissues, even in unforeseen ways, to satisfy safety regulators.
- Standardized manufacturing: Ensuring consistent, high-quality production helps build trust and meets regulatory standards.
- Comprehensive documentation: You’ll need detailed reports on preclinical results, potential risks, and proposed trial protocols.
Navigating these hurdles demands collaboration with regulatory agencies like the FDA or EMA. Only after these steps are satisfied can your nanobots enter human trials, moving closer to transforming cancer treatment.
Developing Accurate Animal Models
Developing accurate animal models is essential for translating nanobot therapies into human clinical trials, yet it remains a significant challenge. You need models that closely mimic human tumors’ complexity, microenvironment, and immune response. Current models often oversimplify cancer, leading to misleading results. For instance, mice with genetically engineered tumors or patient-derived xenografts offer better insights but still fall short of replicating human disease precisely. You must also consider differences in size, metabolism, and physiology between animals and humans. Without refined models, nanobots’ safety, targeting efficacy, and potential side effects can’t be reliably assessed. Incorporating insights from Decoding Slang: Understanding Informal Language Today can help researchers better communicate complex findings across interdisciplinary teams. Overcoming these hurdles requires innovative approaches, like humanized models or advanced bioengineered systems, to guarantee that promising lab results translate into safe, effective treatments in human trials. Additionally, integrating animal models with human-like features can enhance the predictive validity of preclinical studies. Employing innovative bioengineering techniques can further improve the accuracy of these models and bridge the gap between lab research and clinical application. Furthermore, leveraging biomimetic models can provide more realistic environments for studying nanobot interactions and effectiveness. Developing multi-species models may also offer more comprehensive insights into immune responses and therapeutic outcomes.
The Potential of Nanobots to Transform Cancer Surgery
Nanobots hold the promise to revolutionize cancer surgery by enabling highly precise, minimally invasive procedures that target tumors directly while sparing healthy tissue. Imagine guiding tiny robotic agents through your bloodstream to locate and remove cancer cells with pinpoint accuracy. Visualize a swarm of nanobots:
Nanobots could revolutionize cancer surgery with precise, minimally invasive tumor targeting.
- Steering through blood vessels, avoiding healthy tissue, and zeroing in on tumor sites.
- Activating only in acidic tumor microenvironments to release lethal peptides, destroying cancer cells from within.
- Coagulating blood vessels feeding the tumor, effectively starving it and preventing regrowth.
These advancements mean less damage, fewer side effects, and faster recovery. As nanobots become more sophisticated, they could perform complex surgeries inside your body, transforming the way cancer is treated and greatly improving outcomes. Incorporating AI-powered control systems can enhance the precision and adaptability of nanobot operations, making treatments even more effective. Additionally, ongoing research into biocompatible materials ensures that nanobots can operate safely within the human body without adverse reactions. Moreover, blockchain technology could be used to securely track and verify nanobot procedures, increasing trust and transparency in this emerging field.
Harnessing Nanobots for Gene Therapy and Immune Activation
Harnessing nanobots for gene therapy and immune activation offers a promising approach to fight cancer from within. You can deploy nanobots to deliver gene-editing tools directly into cancer cells, correcting mutations or disabling oncogenes. They can also introduce RNA interference molecules to silence tumor-promoting genes. Additionally, nanobots can stimulate your immune system by releasing cytokines like IL-12, boosting immune cells’ ability to attack tumors. These nanobots are designed to target cancer specifically, minimizing damage to healthy tissue. By enhancing immune response and gene correction simultaneously, this strategy offers a dual attack. Advanced nanostructures ensure precise delivery and controlled release, making the therapy more effective. This approach could revolutionize cancer treatment, transforming your body’s defenses into a precise, internal battleground against tumors.
Advanced Targeting Strategies for Selective Cancer Attack
Building on the potential of nanobots to enhance immune responses, precise targeting strategies are vital to guarantee they attack only cancer cells without harming healthy tissue. You can envision nanobots:
- Binding specifically to tumor surface proteins like nucleolin or unique peptides, ensuring they stick only where needed.
- Using oxygen or microenvironment cues to navigate directly into low-oxygen tumor zones, avoiding healthy tissue.
- Unfolding DNA origami structures inside tumors to release potent peptides, activating lethal effects precisely where cancer resides.
These strategies enable nanobots to distinguish cancer from normal cells, reducing side effects. By harnessing such advanced targeting methods, you markedly improve the effectiveness of nanobots in selectively attacking tumors while sparing healthy tissue.
Combining Nanobots With Existing Treatments for Better Outcomes
By combining nanobots with current cancer treatments, you can create more effective therapies that work synergistically. This approach can boost treatment success while reducing side effects, as nanobots target tumors precisely and spare healthy tissue. Ultimately, integrating nanobots with existing methods offers a promising path to better outcomes for patients.
Enhanced Treatment Synergy
Combining nanobots with existing cancer treatments can considerably enhance therapeutic outcomes by targeting tumors more precisely and reducing side effects. You might imagine nanobots guiding chemotherapy directly to cancer cells, minimizing damage to healthy tissue. Or picture nanobots boosting radiotherapy, making it more effective at lower doses. Ultimately, consider nanobots releasing drugs in response to tumor-specific signals, ensuring localized treatment. Specifically:
- Nanobots escort chemotherapy agents, increasing tumor uptake and decreasing systemic toxicity.
- They enhance radiotherapy by delivering radiosensitizers precisely where needed.
- They activate in tumor microenvironments, releasing drugs only in cancerous areas, sparing healthy cells.
This synergy not only amplifies treatment effects but also reduces adverse reactions, making cancer therapy more efficient and patient-friendly.
Minimizing Side Effects
Integrating nanobots with existing cancer treatments offers a promising way to minimize side effects while maintaining or enhancing therapeutic effectiveness. Nanobots can target tumors precisely, delivering drugs directly to cancer cells and reducing damage to healthy tissue. For example, DNA origami nanorobots bind specifically to tumor vascular cells, sparing normal blood vessels. This targeted approach means lower doses of chemotherapy are needed, lessening systemic toxicity. Nanobots can also activate only in the tumor’s acidic environment, preventing collateral damage. When combined with traditional therapies like radiotherapy or surgery, nanobots improve accuracy, reduce complications, and speed recovery. By enhancing selectivity and control, nanobots help you avoid many adverse effects associated with conventional treatments, making cancer therapy safer and more tolerable.
Future Directions and Emerging Technologies in Nanomedicine
Emerging technologies in nanomedicine are pushing the boundaries of cancer treatment beyond traditional approaches. You can imagine nanobots that activate only in the tumor’s acidic microenvironment, sparing healthy tissue. They could be guided precisely by magnetic fields or oxygen gradients, honing in on cancer cells with laser-like accuracy. Visualize DNA origami nanorobots unfolding upon reaching the tumor, exposing lethal peptides, or nanobots delivering thrombin to clot blood vessels and starve tumors. These innovations pave the way for smarter, more targeted therapies. Key future directions include:
- Developing autonomous nanobots capable of on-the-spot decision-making.
- Integrating AI to enhance targeting precision and adapt to tumor changes.
- Combining nanotechnology with immune modulation for all-encompassing cancer eradication.
Ethical and Regulatory Considerations for Nanobot Cancer Therapies

As nanobot cancer therapies move closer to clinical application, ethical and regulatory considerations become increasingly critical. You need to guarantee safety, especially since nanobots target tumors precisely, but unintended effects could harm healthy tissue. Regulatory agencies must develop standards for manufacturing, quality control, and long-term monitoring, addressing potential environmental impacts and bioaccumulation. Ethical concerns include patient consent, privacy, and the risk of misuse or dual-use applications. You also have to contemplate equitable access, avoiding disparities in treatment availability. Transparency in clinical trial results and ongoing safety data is essential to build public trust. Balancing innovation with thorough oversight ensures that nanobot therapies benefit patients without exposing them to unnecessary risks or ethical dilemmas.
Frequently Asked Questions
How Close Are Nanobot Therapies to Clinical Human Trials?
Nanobot therapies are getting closer to clinical trials but haven’t fully reached humans yet. Right now, most research stays in animal studies, showing promising results like tumor reduction and targeted drug delivery. Researchers are working on refining these techniques, addressing safety concerns, and developing better models. You can expect some early human trials to begin in the next few years as scientists validate safety and effectiveness for clinical use.
What Are Potential Side Effects of Nanobots in Humans?
You should be aware that nanobots could cause side effects like immune reactions, inflammation, or unintended damage to healthy tissues. There’s also a risk of toxicity if they accumulate or break down unexpectedly inside your body. While researchers aim to minimize these risks through targeted design, ongoing studies are essential to fully understand safety profiles before these treatments become widely available.
Can Nanobots Target Metastasized or Hard-To-Reach Tumors?
You stand on the brink of a medical revolution where nanobots act like tiny explorers, venturing into the most elusive corners of your body. These microscopic heroes can target metastasized or hard-to-reach tumors by maneuvering through blood vessels, guided by tumor-specific signals. Their precision makes them capable of infiltrating even the most hidden cancer nests, bringing hope for complete treatment and a future where no tumor escapes their grasp.
How Do Nanobots Compare Cost-Wise to Traditional Cancer Treatments?
Nanobots are currently more expensive than traditional cancer treatments because they involve advanced technology, specialized manufacturing, and ongoing research costs. You might find that initial prices are high, but as production scales up and technology matures, costs could decrease. While traditional therapies like chemotherapy are cheaper upfront, nanobots could offer more precise targeting, fewer side effects, and potentially lower long-term healthcare costs, making them a promising investment for future cancer care.
What Regulatory Hurdles Must Be Overcome for Approval?
You need to get past rigorous regulatory hurdles for approval, including demonstrating safety and efficacy. Only 10% of new medical devices reach approval, emphasizing the challenge. You’ll face lengthy clinical trials, detailed safety evaluations, and approval from agencies like the FDA or EMA. Ensuring consistent manufacturing, addressing ethical concerns, and managing potential side effects are essential steps. Overcoming these hurdles will be indispensable to bring innovative nanobot cancer treatments to patients.
Conclusion
You’re on the brink of a revolution in cancer treatment, with nanobots showing promise to reduce tumors by up to 90% in animal studies. Imagine a future where pinpoint precision minimizes side effects and improves survival rates. As researchers overcome current hurdles, the potential for nanobots to transform surgery and therapy grows closer. Stay tuned—this groundbreaking technology could soon change how you fight cancer, making treatments safer, smarter, and more effective than ever before.