Nanomedicine offers promising advances in diabetes care through smart insulin delivery systems that automatically adjust blood sugar levels. These systems use responsive nanomaterials and nanoparticles to monitor glucose and release insulin precisely when needed. They mimic natural insulin response, improving control and reducing injections. Despite challenges like safety and manufacturing, ongoing research shows great progress toward more personalized and effective treatments. Keep exploring to discover how these innovative solutions are transforming diabetes management.
Key Takeaways
- Smart insulin delivery systems utilize responsive nanomaterials and glucose sensors for real-time, automatic blood sugar regulation.
- Nano-encapsulated insulin enhances targeted delivery, stability, and environmental responsiveness, reducing manual injections.
- These systems mimic pancreatic function by releasing insulin dynamically based on blood glucose levels.
- Challenges include ensuring nanoparticle safety, scalable manufacturing, and regulatory approval processes.
- Ongoing research aims to improve biocompatibility, targeting precision, and the overall safety and efficacy of nanomedicine-based insulin therapies.
Understanding Nanomedicine and Its Role in Diabetes Care

Have you ever wondered how tiny particles can revolutionize diabetes treatment? Nanomedicine history shows how scientists have harnessed nanoparticles to improve healthcare, especially for chronic conditions like diabetes. These minuscule materials enable targeted drug delivery, reducing side effects and improving insulin efficiency. However, using nanotechnology in medicine isn’t without regulatory challenges. Authorities require rigorous testing to guarantee safety, efficacy, and quality control, which can slow down innovation. As you explore nanomedicine’s role in diabetes care, it’s important to understand these hurdles and advancements. Researchers continue refining nanotech solutions to make treatments more precise, safe, and accessible. Ultimately, nanomedicine’s history and regulatory landscape shape how quickly these groundbreaking therapies can reach and benefit patients like you. AI safety measures are also crucial as these technologies develop and become more integrated into healthcare systems.
Types of Smart Insulin Delivery Systems Utilizing Nanotechnology
Smart insulin delivery systems using nanotechnology include responsive glucose sensors and nano-encapsulated insulin. These innovations automatically adjust insulin release based on your blood sugar levels, improving control and convenience. Exploring how these systems work can help you understand their potential to transform diabetes management. Incorporating mindfulness techniques into daily routines can also support better health and stress management alongside medical advancements.
Responsive Glucose Sensors
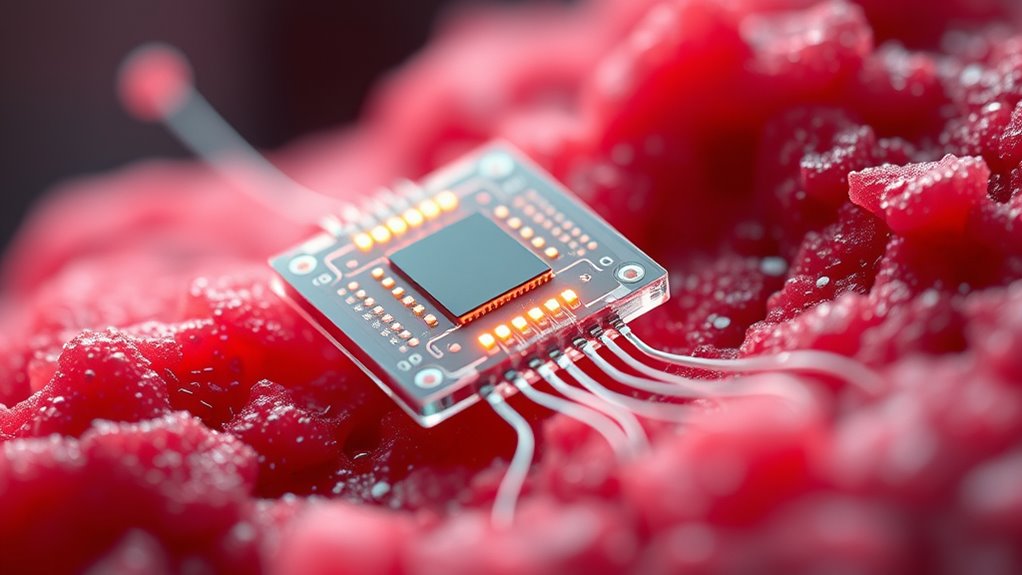
How do responsive glucose sensors revolutionize insulin delivery in diabetes management? They enable real-time monitoring and automatic adjustments, reducing manual interventions. Advances in biosensor innovation allow for highly sensitive detection of glucose levels, providing accurate data quickly. Nanocarrier design plays a pivotal role by improving sensor responsiveness and stability, ensuring consistent performance. These sensors detect glucose fluctuations and trigger insulin release precisely when needed, mimicking the body’s natural regulation. With nanotechnology, sensors become more compact, less invasive, and more durable, enhancing patient comfort and compliance. This integration of nanomaterials improves the overall efficiency of insulin delivery systems, making diabetes management safer, more effective, and personalized. Ultimately, responsive glucose sensors represent a significant leap toward closed-loop, smart insulin systems.
Nano-Encapsulated Insulin
Nano-encapsulated insulin systems leverage nanotechnology to improve insulin delivery by protecting the hormone and enabling targeted release. These systems use nanoparticle synthesis to create nanocarriers that can navigate to specific tissues, such as the liver or muscle. Nanocarrier targeting enhances precision, reducing side effects and optimizing glucose regulation. The nanocarriers release insulin in response to environmental cues, like glucose levels, making the delivery smarter and more effective.
| Feature | Benefit |
|---|---|
| Nanoparticle synthesis | Ensures stable, uniform nanocarriers |
| Nanocarrier targeting | Improves delivery accuracy to specific tissues |
| Responsive release | Releases insulin only when needed |
| Enhanced stability | Protects insulin from degradation |
| Controlled release | Provides sustained glucose control |
How Nanoparticles Enhance Insulin Stability and Release
Nanoparticles help protect insulin from degradation, ensuring it stays effective longer in your body. They also enable controlled release, so insulin is delivered steadily rather than all at once. This combination improves treatment stability and mimics natural insulin patterns more closely. Additionally, advanced delivery systems can be tailored to individual patient needs, further enhancing therapy effectiveness.
Improved Insulin Protection
Nanomedicine offers a powerful way to protect insulin from degradation and guarantee its effective release. By optimizing nanoparticle synthesis, you can create protective carriers that shield insulin from enzymatic breakdown and environmental factors. These nanoparticles improve drug delivery pathways, ensuring insulin stays stable until it reaches its target. Here are three ways they enhance protection:
- Encapsulation prevents insulin from exposure to harsh conditions.
- Surface modifications improve resistance to enzymatic degradation.
- Controlled degradation rates ensure timely release without premature breakdown.
This approach not only preserves insulin’s bioactivity but also ensures it remains effective over extended periods. With these advancements, you’re better equipped to design resilient delivery systems that optimize insulin stability, making diabetes management safer and more reliable.
Controlled Release Mechanisms
Have you ever wondered how insulin can be released steadily over time despite the body’s complex environment? That’s where controlled release mechanisms shine. Nanoparticles, crafted through precise nanoparticle synthesis, can be engineered to respond to specific stimuli, ensuring consistent insulin delivery. They optimize drug delivery pathways by protecting insulin from degradation and releasing it gradually. This controlled release reduces the risk of sudden glucose spikes and mimics natural insulin patterns.
| Insulin Stability | Release Timing | Patient Comfort |
|---|---|---|
| Enhanced protection | Steady, predictable | Fewer injections |
| Reduced degradation | Mimics natural rhythms | Less discomfort |
| Improved efficacy | Better glucose control | Increased confidence |
Responsive Nanomaterials for Glucose-Triggered Insulin Release

Responsive nanomaterials are designed to release insulin precisely when blood glucose levels rise, enabling a more effective and automatic management of diabetes. To achieve this, you need to focus on:
- Biosensor integration, which allows nanomaterials to detect glucose fluctuations in real time.
- Nanoparticle synthesis, creating structures that respond swiftly to glucose changes.
- Tailoring the material’s responsiveness, ensuring insulin release occurs only at specific glucose concentrations.
These strategies enable your nanomaterials to function as smart sensors, activating insulin release when needed. The integration of biosensors with nanomaterials ensures accurate detection, while advanced nanoparticle synthesis improves responsiveness. This synergy results in a system that mimics pancreatic function, providing a seamless, automatic therapy for diabetics.
Advantages of Nanoscale Devices Over Traditional Insulin Therapies
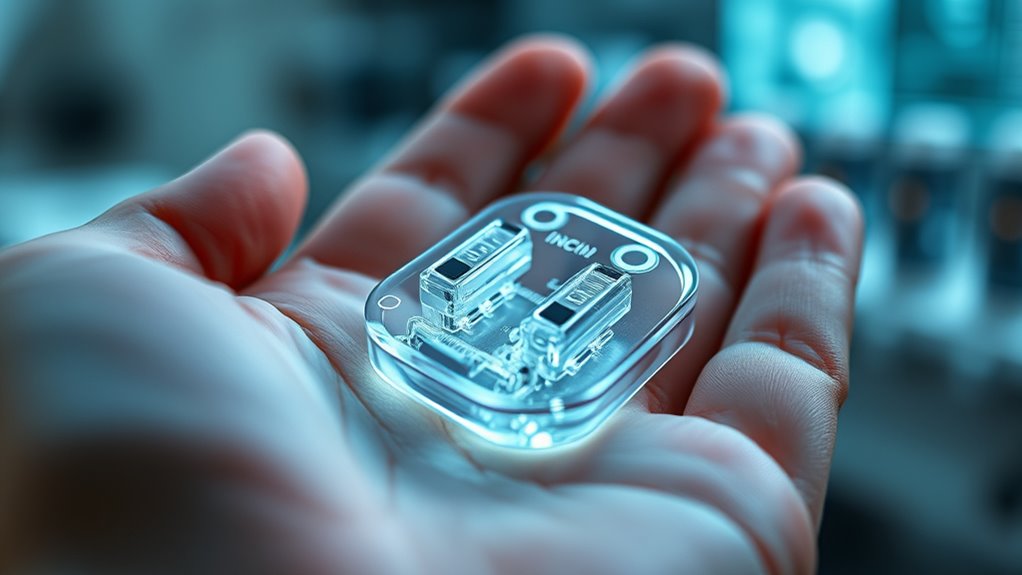
Nanoscale devices offer significant advantages over traditional insulin therapies by providing precise, on-demand glucose regulation. They respond quickly to fluctuating blood sugar levels, reducing risks of hyper- or hypoglycemia. Unlike injections, these systems can minimize multiple daily doses, enhancing comfort and compliance. However, nanoparticle toxicity remains a concern, as unintended interactions could harm tissues. Ethical considerations also arise around long-term safety and informed consent. To illustrate, here’s a comparison:
| Aspect | Traditional Therapy | Nanoscale Devices |
|---|---|---|
| Glucose regulation | Manual injections | Automated, on-demand response |
| Patient compliance | Variable, discomfort | Improved, less invasive |
| Safety concerns | Few, well-understood | Nanoparticle toxicity risks |
| Ethical considerations | Minimal | Data privacy, long-term effects |
| Response time | Slow | Rapid, real-time adjustments |
Additionally, ongoing research into biocompatible materials aims to mitigate toxicity risks and enhance the safety profile of these innovative systems.
Current Challenges and Limitations in Developing Nanomedicine-Based Insulin Systems

Despite the promising advantages of nanomedicine-based insulin systems, several hurdles remain before they can become widely available. First, nanoparticle toxicity raises safety concerns, as some materials may cause adverse reactions or long-term health issues. Second, manufacturing scalability poses challenges; producing consistent, high-quality nanocarriers in large quantities is complex and costly. Third, ensuring precise control over drug release and stability within the body remains difficult, risking inconsistent insulin delivery. These issues hinder regulatory approval and clinical adoption. Overcoming nanoparticle toxicity involves developing safer materials, while scalable manufacturing requires advanced production techniques. Addressing these challenges is *vital* to translating nanomedicine innovations from research to real-world diabetes management. Additionally, fostering creative problem-solving approaches can accelerate the development of safer and more efficient nanomedicine systems.
Future Perspectives and Emerging Trends in Nanomedicine for Diabetes
Emerging trends in nanomedicine for diabetes are poised to transform disease management by integrating advanced materials and innovative delivery systems. Researchers are exploring new nanocarriers that improve targeting and reduce side effects. However, nanoparticle toxicity remains a concern, requiring thorough safety assessments before widespread use. Future developments aim to enhance biocompatibility and minimize adverse reactions. Additionally, regulatory hurdles must be addressed to facilitate clinical translation; clear guidelines and standardized testing are essential. You’ll see increased focus on scalable manufacturing processes and long-term stability of nanomedicines. As these trends evolve, you can expect more personalized and efficient insulin delivery solutions. Ultimately, overcoming safety and regulatory challenges will be key to accessing the full potential of nanomedicine in diabetes management.
Clinical Trials and Real-World Applications of Smart Nanoinsulin Devices

Clinical trials of smart nanoinsulin devices are rapidly advancing, bringing these innovative systems closer to real-world use. As you follow these developments, consider key factors shaping their success:
- Researchers are carefully evaluating nanoparticle toxicity to guarantee safety during long-term use.
- Clinical data demonstrate improved glycemic control, showing promise for patient outcomes.
- Regulatory approval remains a hurdle, with agencies requiring exhaustive safety and efficacy evidence before widespread adoption.
- The biocompatibility of nanoparticles is continually assessed to ensure minimal adverse reactions in patients.
These trials help address concerns about nanoparticle toxicity, guaranteeing devices are safe for everyday use. Achieving regulatory approval is vital for bringing smart nanoinsulin systems from lab settings to clinics. As these steps unfold, you can expect more tailored, efficient insulin delivery solutions that transform diabetes management.
Frequently Asked Questions
How Do Nanomedicine-Based Systems Adapt to Individual Patient Needs?
You benefit from nanomedicine-based systems through personalized dosing tailored to your unique needs. Adaptive sensors continuously monitor your glucose levels, allowing the system to modify insulin delivery in real-time. This dynamic approach ensures better blood sugar management, reduces the risk of hypo- or hyperglycemia, and enhances your overall quality of life. By responding to your body’s signals, these systems provide a more precise and effective diabetes treatment.
What Are the Potential Long-Term Effects of Nanomaterials in Diabetes Treatment?
You should consider that the potential toxicity of nanomaterials might cause long-term health issues, like immune reactions or cellular damage, as they accumulate in your body. Additionally, the environmental impact of manufacturing and disposing of nanomaterials could harm ecosystems. While nanomedicine offers promising benefits, ongoing research is essential to understand and mitigate these long-term effects, ensuring your safety and environmental sustainability.
How Cost-Effective Are Nanotechnology-Driven Insulin Delivery Methods?
You’ll find nanotechnology-driven insulin delivery methods are becoming increasingly cost-effective as research advances and manufacturing scales up. A thorough cost analysis shows potential savings over traditional treatments, especially with reduced hospital visits and improved glucose control. Funding strategies like government grants and public-private partnerships can accelerate development and adoption, making these innovative systems more accessible and affordable for you in the long run.
What Regulatory Hurdles Exist for Approving Nanomedicine for Diabetes?
You face significant regulatory hurdles for approving nanomedicine for diabetes, mainly involving rigorous regulatory approval processes. Authorities require thorough safety assessments to guarantee the nanomaterials are safe for long-term use, which can be complex due to their novel properties. You must also demonstrate consistent manufacturing quality and efficacy. Managing these regulations demands comprehensive data and close collaboration with regulatory agencies to meet all safety and efficacy standards.
How Can Nanomedicine Improve Insulin Therapy in Type 1 Versus Type 2 Diabetes?
Imagine a world where your insulin delivery is perfectly timed; nanomedicine makes this possible. You benefit from nanoparticle targeting and advanced insulin nanocarriers that respond to blood sugar levels. For type 1 diabetes, these systems provide precise, on-demand insulin, reducing hypoglycemia risks. In type 2, they enhance existing treatments by improving insulin sensitivity and delivery, making therapy more efficient and personalized.
Conclusion
As you explore nanomedicine’s role in diabetes care, it’s fascinating how tiny innovations can have such a big impact. The coincidence of advanced materials and smart technology promises more precise insulin delivery, ultimately transforming lives. While challenges remain, the emerging trends suggest that your future might include seamless, responsive treatments tailored just for you. It’s an exciting time where science and hope intersect, making better diabetes management not just possible, but inevitable.