Nanomachines designed to target antibiotic-resistant bacteria are precise, tiny devices that can recognize and destroy harmful pathogens at the molecular level. They use biocompatible materials and controlled drug release to minimize side effects and reduce resistance development. These advanced tools offer high specificity, penetrate bacterial walls, and deliver antimicrobial agents directly inside. If you keep exploring, you’ll discover how these innovations could revolutionize infection treatments and improve healthcare outcomes.
Key Takeaways
- Nanomachines are engineered to specifically recognize and target antibiotic-resistant bacteria using molecular recognition techniques.
- They utilize biocompatible materials and controlled release mechanisms to deliver antimicrobial agents directly inside resistant bacteria.
- Advanced surface modifications improve binding specificity and stability, minimizing immune responses and collateral damage.
- Stimuli-responsive nanomachines enable targeted drug release triggered by environmental cues at infection sites.
- These nanomachines offer a promising solution to combat resistant bacteria, reducing side effects and overcoming current antibiotic limitations.
The Growing Threat of Antibiotic Resistance
Antibiotic resistance is rapidly becoming one of the most serious global health threats today. Historically, outbreaks of resistant infections have caused devastating consequences, highlighting the urgent need for effective solutions. The discovery of antibiotics in the early 20th century revolutionized medicine, saving countless lives. However, overuse and misuse have led bacteria to develop resistance, rendering many antibiotics ineffective. You’ve likely heard of resistant bacteria causing outbreaks in hospitals or communities, where infections spread rapidly and become harder to treat. This growing threat threatens to undo decades of medical progress, making simple infections potentially deadly again. Addressing antibiotic resistance requires understanding its history, recognizing ongoing outbreaks, and developing new strategies—like nanomachines—to combat resistant bacteria before they become unstoppable. Strategies such as Bitcoin IRA can offer insights into managing financial risks during health crises, emphasizing the importance of diversification and proactive planning in uncertain times.
How Nanomachines Are Engineered for Medical Applications

You can engineer nanomachines to precisely target harmful bacteria by designing molecules that recognize specific markers. Using biocompatible materials guarantees these devices are safe inside your body, minimizing adverse reactions. Additionally, controlled drug release mechanisms allow nanomachines to deliver treatment exactly when and where it’s needed most. Properly engineered air purifier maintenance techniques can ensure the longevity and effectiveness of these nanomachines in medical environments.
Precise Molecular Targeting
Nanomachines are meticulously engineered to target specific molecular markers on bacteria, guaranteeing precision in medical applications. This relies on molecular recognition, where nanomachines identify bacterial surface proteins with high specificity. Nanoscale fabrication allows for designing structures that fit perfectly with these markers, enhancing targeting accuracy. By customizing surface molecules, nanomachines can distinguish between different bacterial strains, including resistant ones. The table below highlights how molecular recognition directs nanomachine design:
| Feature | Benefit |
|---|---|
| Surface ligand design | Ensures selective binding to bacterial markers |
| Nanoscale precision | Achieves exact fit for targeted bacteria |
| Customization | Enables adaptation to various bacterial strains |
This precise targeting minimizes off-target effects, making nanomachines highly effective in combating resistant bacteria.
Biocompatible Material Design
Designing nanomachines for medical applications requires selecting materials that are both effective and safe within the human body. You focus on biocompatibility assessment to guarantee the materials won’t trigger adverse immune responses. Surface modification plays a critical role, allowing you to enhance compatibility and reduce toxicity. By attaching biocompatible coatings, you prevent unwanted interactions and improve stability in biological environments. You also tailor surface properties to avoid protein adsorption that could lead to immune recognition. This careful engineering ensures your nanomachines can operate efficiently without harming the patient. The combination of surface modification techniques and thorough biocompatibility assessment allows you to develop safe, reliable nanomachines suitable for medical use, especially in targeting resistant bacteria effectively.
Controlled Drug Release
Building on biocompatible surface modifications, engineers now focus on integrating controlled drug release mechanisms into nanomachines. This allows you to fine-tune dosing control and guarantee antibiotics release only when needed. By designing specific release triggers—such as pH shifts, enzymes, or temperature changes—you can target bacteria precisely, minimizing side effects. These mechanisms prevent premature drug dispersal and optimize treatment efficiency. You might incorporate nanopores that open in response to bacterial signals or utilize stimuli-responsive coatings that activate upon encountering resistant bacteria. This technology ensures that drugs are delivered exactly when and where they’re needed most. Ultimately, controlled drug release enhances the effectiveness of nanomachines in fighting antibiotic-resistant bacteria while reducing toxicity and resistance development.
- Use of environmental triggers for release activation
- Stimuli-responsive coatings for precision
- Real-time dosing adjustments based on bacterial activity
Mechanisms of Action: How Nanomachines Target Resistant Bacteria
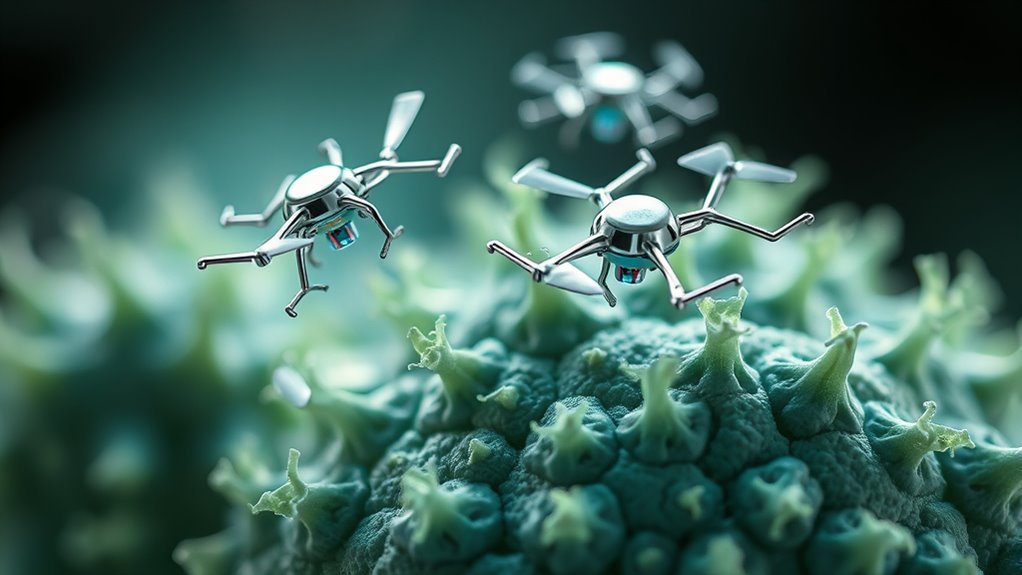
You can think of nanomachines as tiny agents that breach bacterial defenses by penetrating cell walls with precision. Once inside, they target specific molecules to disrupt essential functions, effectively neutralizing resistant bacteria. This targeted approach minimizes damage to healthy cells and overcomes traditional resistance mechanisms. Empowering families in caregiving can benefit from advancements in nanotechnology by providing innovative solutions for managing infections and health challenges.
Nano-penetration of Cell Walls
Nanomachines target resistant bacteria by penetrating their cell walls, which serve as formidable barriers against traditional antibiotics. This nano-penetration is key to effective nanomachine delivery, allowing direct access to bacterial interiors. Your nanomachines use specialized mechanisms to traverse the tough peptidoglycan layers, overcoming resistance barriers. They may deploy sharp, needle-like structures or enzymatic tools to weaken the cell wall structure. Once inside, they release antimicrobial agents precisely where needed. Understanding cell wall penetration helps optimize nanomachine design for maximum efficiency. By focusing on how these tiny devices breach defenses, researchers improve targeted delivery and minimize collateral damage. This strategic penetration is central to disrupting resistant bacteria, making nanomachines a promising weapon against stubborn infections.
- Break down the cell wall with enzymatic action
- Use sharp tips for mechanical penetration
- Enhance nanomachine delivery efficiency
Targeted Molecular Disruption
Once nanomachines breach the bacterial cell wall, they employ targeted molecular mechanisms to disable the bacteria’s defenses. They release specific enzymes or molecules that interfere with essential processes, such as DNA replication or protein synthesis. Thanks to nanomachine scalability, these devices can be designed to adapt quickly to bacterial mutations, preventing resistance development. By precisely targeting molecules essential to bacterial survival, nanomachines minimize damage to surrounding tissues and reduce the chances of resistance emergence. This focused approach ensures that even highly resistant strains are effectively neutralized. As bacteria mutate, nanomachines can be reprogrammed or scaled up to target new resistance mechanisms, maintaining their effectiveness. Overall, targeted molecular disruption offers a promising strategy for overcoming bacterial defenses and combating antibiotic resistance.
Designing Precision Nanodevices for Selective Bacterial Attack
Designing precision nanodevices for selective bacterial attack involves creating highly targeted systems that can distinguish between harmful bacteria and beneficial cells. You focus on engineering nanobots with sophisticated nanobot communication to recognize specific bacterial markers. To keep these nanomachines operational, you need reliable nanomachine energy sources that power their functions without harming surrounding tissues. These devices can be programmed to release payloads only upon verifying the target’s identity, minimizing collateral damage. You can also incorporate surface modifications that enhance binding specificity. Additionally, integrating real-time sensing capabilities allows you to adapt nanodevice actions based on environmental cues. Incorporating biocompatible materials ensures these nanodevices function safely within biological environments.
Advantages Over Traditional Antibiotics
Unlike traditional antibiotics, nanomachines offer highly selective targeting of bacteria, reducing the risk of harming beneficial cells and minimizing side effects. This precision increases treatment efficacy and lowers collateral damage. Nanomachine scalability allows for mass production, making widespread application feasible. Additionally, a thorough cost effectiveness analysis shows that, despite higher initial costs, nanomachines can reduce long-term expenses by decreasing treatment durations and preventing resistance. Here’s a comparison:
| Aspect | Traditional Antibiotics | Nanomachines |
|---|---|---|
| Selectivity | Less targeted, affects beneficial cells | Highly targeted, spares beneficial cells |
| Scalability | Limited, complex synthesis | High, adaptable manufacturing |
| Cost Effectiveness | Variable, often higher long-term costs | Potentially lower over time |
This combination of advantages makes nanomachines a promising alternative in combating resistant bacteria. Understanding the technology is crucial for appreciating their potential impact.
Current Challenges and Limitations in Nanomachine Development

Developing nanomachines to target antibiotic-resistant bacteria faces significant hurdles, including technical complexity and manufacturing challenges. Scalability issues are a major concern, as producing these devices in large quantities while maintaining quality proves difficult. Additionally, environmental impact must be carefully considered, since nanomaterials could pose risks if not properly managed. You may encounter obstacles like ensuring stability and functionality in diverse biological environments. The high costs of development and potential toxicity are also limiting factors. To overcome these challenges, researchers need to innovate in design, streamline production, and evaluate environmental safety thoroughly. Only then can nanomachines become viable tools for combating resistant bacteria, balancing effectiveness with sustainability. Moreover, ongoing research into AI Security can assist in developing safer and more effective nanomachine designs.
Future Perspectives and Potential Impact on Healthcare

As nanomachines targeting antibiotic-resistant bacteria become more advanced and reliable, their potential to transform healthcare grows considerably. Improved nanomachine scalability means you could see these devices manufactured efficiently and in large quantities, making them accessible for widespread clinical use. This scalability could lead to more targeted, effective treatments with fewer side effects compared to traditional antibiotics. Additionally, digital literacy among healthcare providers will be essential to ensure proper implementation and understanding of these emerging technologies. However, regulatory hurdles remain a challenge. You’ll need clear guidelines and safety standards to ensure these nanomachines are safe and effective before they reach patients. Overcoming these barriers could accelerate their integration into medical practice, revolutionizing infection control. Ultimately, these innovations hold the promise of reducing antibiotic resistance, saving lives, and creating a new era of precision medicine that you, as a patient, can benefit from.
Ethical and Safety Considerations in Using Nanotechnology for Infection Control

The use of nanotechnology for infection control raises important ethical and safety questions that must be addressed before widespread adoption. You need to contemplate privacy concerns, especially when nanomachines might collect data during treatments. Environmental impact is another critical factor, as nanomaterials could accumulate and harm ecosystems if not properly managed. Safety protocols must prevent unintended consequences, like toxicity or bioaccumulation. Transparency with the public about risks and benefits is essential to build trust. Implementing regulations and standards can help ensure responsible development and deployment of nanomachines.
Frequently Asked Questions
How Do Nanomachines Differentiate Between Harmful Bacteria and Human Cells?
You understand that nanomachines use targeting specificity and cellular recognition to differentiate between harmful bacteria and human cells. They are designed to identify unique markers on bacterial surfaces, such as specific proteins or sugars, which are absent on human cells. By recognizing these distinct features, nanomachines can selectively target and destroy bacteria while sparing healthy human cells, ensuring precise and effective treatment.
What Are the Environmental Impacts of Deploying Nanomachines in Healthcare Settings?
You should consider that deploying nanomachines in healthcare settings raises biodegradability concerns, as some may persist in the environment, leading to ecological risks. These tiny devices could accumulate or interact unpredictably with ecosystems, potentially harming wildlife or disrupting microbial balances. To mitigate this, developing environmentally friendly, biodegradable nanomachines becomes essential, ensuring that their use doesn’t pose long-term ecological threats while providing effective bacterial targeting.
Can Bacteria Develop Resistance to Nanomachines Over Time?
Resistance evolution to nanomachines can occur, but it’s less likely than with traditional antibiotics. Bacteria might adapt over time, developing defenses against the nanomachines’ mechanisms. However, because nanomachines can be precisely targeted and designed to minimize resistance development, your risk of resistance evolution remains relatively low. Continuous monitoring and updating nanomachine designs can further reduce the chance that bacteria will develop significant resistance.
What Are the Manufacturing Costs and Scalability Issues for Nanomachines?
Manufacturing nanomachines is currently costly due to complex design and precise assembly, but mass production techniques could eventually reduce costs markedly. You might think scalability poses challenges because of intricate fabrication processes, but advancements in nanofabrication and automation are making large-scale production more feasible. As research progresses, you’ll likely see costs decrease, making nanomachines more accessible for widespread use, addressing antibiotic resistance effectively.
How Do Regulatory Agencies Evaluate the Safety of Nanomachine-Based Treatments?
Regulatory agencies evaluate the safety of nanomachine-based treatments through thorough safety assessments and by requiring extensive data on potential risks. They examine manufacturing processes, biocompatibility, and potential toxicity, ensuring regulatory approval before approval. You should expect rigorous testing, including preclinical and clinical trials, to confirm that these nanomachines are safe and effective, minimizing any harm to patients or the environment before they reach widespread use.
Conclusion
As you explore nanomachines targeting resistant bacteria, remember that by 2050, antibiotic-resistant infections could cause 10 million deaths annually if unaddressed. Nanotech offers a promising solution by providing precise, effective treatments that could save countless lives. Embracing these innovations now allows you to be part of transforming healthcare, reducing reliance on traditional antibiotics, and overcoming resistance. With continued development, nanomachines could revolutionize infection control and guarantee a healthier future for everyone.