Nanotech is revolutionizing diabetes management by offering highly sensitive, noninvasive glucose monitoring options like wearable sensors, smart contact lenses, and sweat analyzers. It also enables precise, feedback-controlled insulin delivery through nanocarriers that respond to blood sugar levels. These advancements aim to make diabetes care more comfortable, accurate, and tailored to your needs. Keep exploring to discover how nanotechnology is shaping the future of diabetes treatment and how it could benefit you.
Key Takeaways
- Nanotech-enhanced electrodes improve glucose detection sensitivity and response time in diabetes monitoring devices.
- Wearable nanobiosensors enable noninvasive, pain-free glucose measurement through sweat, tears, or interstitial fluid.
- Nanocarriers facilitate smart, feedback-controlled insulin delivery, mimicking pancreatic function for better glucose regulation.
- Advanced nanomaterials increase sensor durability, biocompatibility, and resistance to biofouling for long-term use.
- Integration of nanotechnology with AI and closed-loop systems advances personalized, real-time diabetes management solutions.
Advances in Nanomaterial-Modified Electrodes for Continuous Glucose Detection

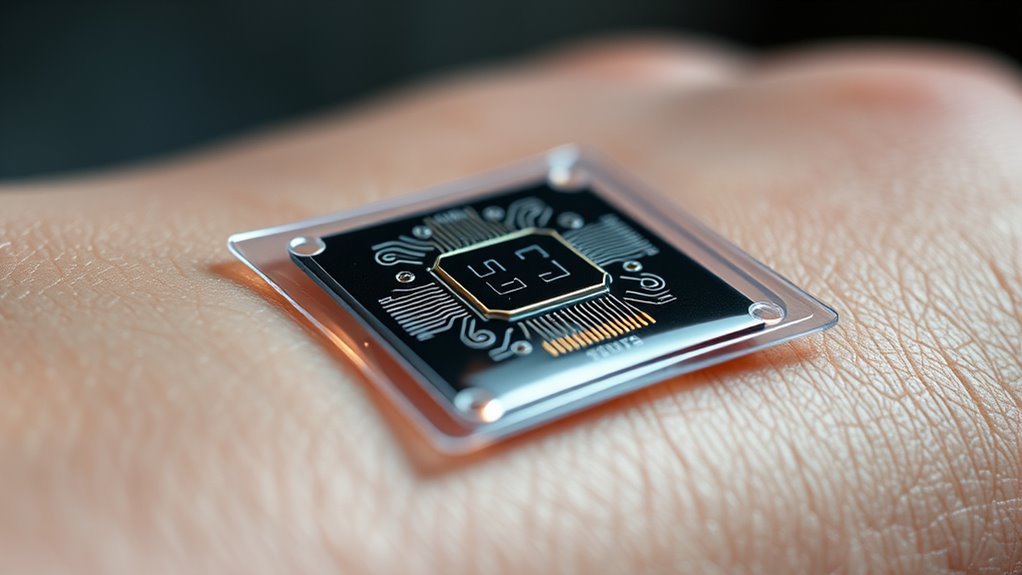
Nanomaterial-modified electrodes have revolutionized continuous glucose detection by markedly enhancing sensitivity and lowering detection limits. You benefit from improved electron transfer capabilities provided by materials like carbon nanotubes and graphene, which enable near-real-time, accurate readings across a broad glucose range. These nanostructures increase the electrode’s surface area, allowing more enzyme immobilization and better signal transduction. Metal nanoparticles, such as gold and platinum, act as catalysts, further amplifying signals and speeding response times. Surface modifications like polymer brushes or PEGylation improve biocompatibility and reduce fouling, extending sensor lifespan. The integration of these nanomaterials into flexible, wearable platforms makes continuous monitoring more reliable, less invasive, and suitable for real-world use. Additionally, biocompatibility enhancements are crucial for long-term implantation and consistent performance. Incorporating nanostructure stability ensures that sensors maintain their functionality over extended periods, which is vital for effective long-term glucose tracking outside clinical settings. This progress paves the way for more precise, long-term glucose tracking outside clinical settings. Floating on Water
Noninvasive and Minimally Invasive Nanobiosensing Modalities
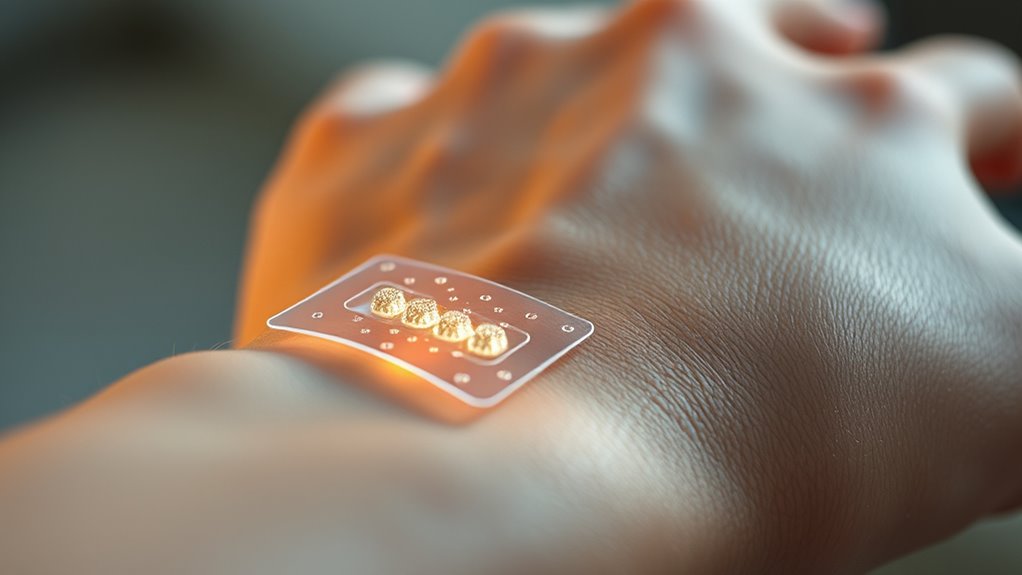
Building on advances in nanomaterial-enhanced electrodes, researchers are now focusing on noninvasive and minimally invasive approaches to monitor glucose levels. You can use nanobiosensors embedded in wearable devices like smart contact lenses, patches, or sweat sensors, which detect glucose in tears, sweat, or saliva without pain. Nanomaterials such as carbon nanotubes and quantum dots improve optical and electrochemical signals, enabling rapid, accurate readings. Painless microneedle arrays made with nanostructured materials sample interstitial fluid with minimal discomfort, providing continuous data. These minimally invasive techniques are increasingly being refined to enhance patient comfort and compliance. Transdermal sensors utilizing near-infrared light and nanomaterials exploit skin transparency windows for noninvasive measurement. Nanomaterials enhance the sensitivity and specificity of these sensors, making real-time monitoring more reliable. Additionally, ongoing research focuses on enhanced biocompatibility to reduce potential adverse reactions and improve long-term device stability. As the technology progresses, smart wearables are becoming more integrated and capable of providing comprehensive health data seamlessly. These innovations allow for real-time glucose monitoring outside clinical settings, making diabetes management more comfortable, accessible, and less burdensome.
Smart Nanocarriers for Feedback-Controlled Insulin Delivery

Smart nanocarriers enable precise, feedback-controlled insulin delivery by responding directly to glucose levels. They release insulin only when needed, mimicking natural pancreatic function. These nanocarriers often use glucose-sensitive materials like phenylboronic acid or enzyme-triggered systems that convert glucose to signals, prompting insulin release. This approach reduces hypoglycemia risk and improves glucose stability. Additionally, ongoing research into biocompatible materials aims to enhance the safety and efficacy of these systems. Innovations in material safety are crucial for clinical adoption. Incorporating advanced nanotechnology techniques can further optimize device performance. The development of these systems relies heavily on understanding material interactions at the nanoscale to ensure stability and responsiveness. Understanding industry trends helps guide research and commercialization strategies. Here’s a quick comparison:
| Nanocarrier Type | Key Feature |
|---|---|
| Phenylboronic acid-based | Reversibly binds glucose, releasing insulin when levels rise |
| Enzyme-triggered (GOx) | Converts glucose to H2O2 or acid, actuating insulin release |
| pH-sensitive | Responds to local pH changes from glucose oxidation |
| Redox-sensitive | Uses redox reactions to control insulin release |
These systems promise smarter, more responsive diabetes management, moving closer to an artificial pancreas.
Fabrication Strategies for Durable and Biocompatible Nano-Glucose Sensors
Creating durable and biocompatible nano-glucose sensors requires careful attention to fabrication strategies that guarantee long-term stability and safe implantation. You should select materials like carbon nanomaterials, metal nanoparticles, or metal-organic frameworks that resist corrosion and fouling. Surface functionalization, such as PEGylation or polymer brushes, minimizes immune response and reduces biofouling, extending sensor lifespan. Incorporate nanostructuring techniques to enhance adhesion and mechanical robustness, ensuring sensors withstand physiological conditions. Utilizing scalable micro/nanopatterning and flexible electronics allows for consistent manufacturing and integration into wearable platforms. Ensuring biocompatibility involves rigorous testing of surface coatings and nanomaterials to prevent toxicity. By focusing on these strategies, you’ll develop sensors that are both stable over time and safe for long-term implantation, advancing continuous glucose monitoring.
Overcoming Challenges: Clinical Validation and Future Directions in Nano-Enabled Diabetes Care

Despite significant advancements in nanotechnology for diabetes management, clinical validation remains a major hurdle before widespread adoption. You need rigorous testing across diverse populations to confirm accuracy, reliability, and safety. Many promising nanosensors show excellent results in lab or small trials but struggle with reproducibility and consistency in real-world settings. Long-term biocompatibility, immune responses, and sensor stability are ongoing concerns that require extensive evaluation. Additionally, regulatory approval processes demand standardized metrics and large-scale clinical trials, which can be costly and time-consuming. Looking ahead, integrating nanotech with AI and closed-loop systems offers personalized, predictive management. Focused efforts on scalable manufacturing, safety profiling, and validation will be critical to translating these innovations from research to routine clinical use, ultimately transforming diabetes care. Furthermore, regulatory compliance is essential to ensure that nano-enabled devices meet safety standards and gain approval for clinical deployment.
Frequently Asked Questions
How Do Nanomaterials Improve the Specificity of Glucose Sensors?
Nanomaterials improve the specificity of glucose sensors by providing high surface area and precise surface chemistry, which allows for better immobilization of enzymes like glucose oxidase. This enhances selectivity by reducing interference from other substances. Additionally, nanostructured supports create a more stable environment for enzymes, maintaining their activity over time, and nanoscale modifications enable targeted interactions with glucose molecules, resulting in more accurate and specific detection.
What Are the Main Safety Concerns for Long-Term Implantable Nanodevices?
While the promise of long-term implantable nanodevices shines brightly, you should be aware of their subtle safety concerns. They might encounter the body’s gentle immune responses or gradual surface changes that could affect performance over time. Additionally, there’s the importance of ensuring nanomaterials remain biocompatible, avoiding unintended tissue interactions, and addressing potential toxicity. Ongoing research endeavors to harmonize these devices with your body’s natural rhythms, ensuring safe, reliable monitoring.
How Does Tissue Penetration Limit Optical Glucose Sensing Accuracy?
Tissue penetration limits optical glucose sensing accuracy because light must pass through skin and tissues, which scatter and absorb photons, reducing signal strength and clarity. This scattering causes signal distortion, making it harder to accurately measure glucose levels. Additionally, variations in tissue thickness, pigmentation, and hydration affect light transmission, leading to inconsistent readings. These factors collectively hinder reliable, precise optical measurements, especially when trying to monitor glucose non-invasively through skin or tears.
Can Nanocarriers Fully Replace Traditional Insulin Administration?
Nanocarriers can’t fully replace traditional insulin administration yet, but they show promising potential. You might benefit from nanocarrier systems that deliver insulin in response to glucose levels, offering more precise, feedback-controlled dosing. However, challenges like long-term stability, biocompatibility, and regulatory approval still need addressing. As research advances, these nanocarriers could become a complementary or alternative option, reducing injections and improving blood sugar management.
What Regulatory Hurdles Exist for Commercializing Nano-Based Glucose Monitors?
You face formidable federal, financial, and formulary hurdles when commercializing nano-based glucose monitors. Regulatory agencies demand rigorous research, reliable results, and robust safety data to guarantee patient protection and product precision. You must navigate nuanced pathways, satisfy stringent standards, and secure significant support, all while demonstrating long-term biocompatibility and accuracy. Overcoming these obstacles requires patience, perseverance, and precise planning to successfully bring groundbreaking nanosensors from laboratory to life.
Conclusion
As you explore the world of nanotech in diabetes care, you’ll find that these tiny innovations gently pave the way for smarter, more comfortable monitoring. With ongoing advances, your journey toward seamless glucose management becomes less intimidating and more hopeful. Embrace the promise of nanomaterials and nanobiosensing—they quietly transform the future, making diabetes care not just easier, but almost effortless. The future’s gentle whispers hint at a new dawn for your health and well-being.









