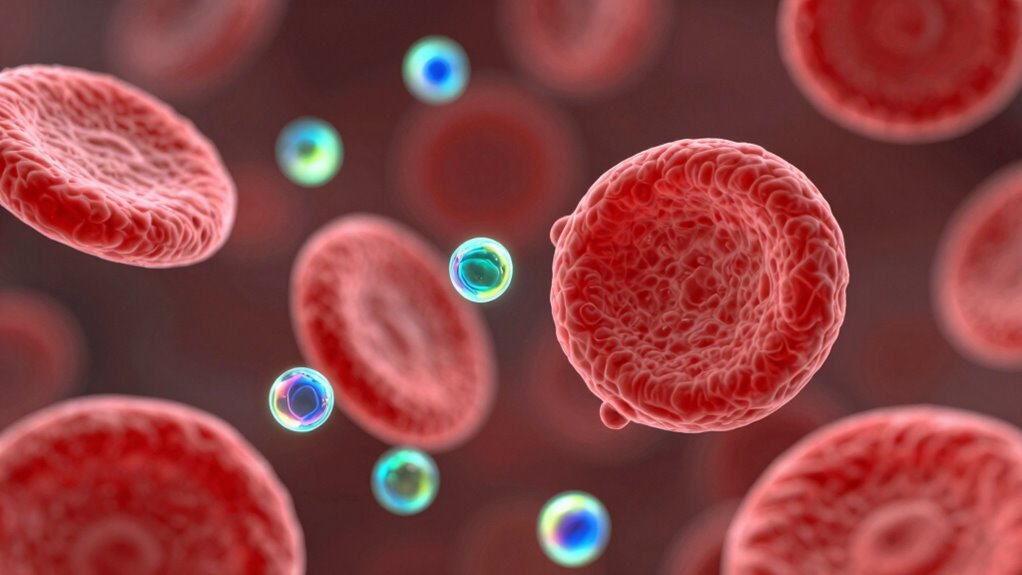
Nanomedicine uses tiny particles, usually between 1-100 nanometers, that travel through your bloodstream to diagnose, deliver drugs, or treat illnesses with high precision. Their small size allows them to navigate biological barriers, target specific cells, and reduce side effects. By customizing surface properties and using targeting ligands or stimuli, these nanocarriers improve treatment effectiveness. To discover how this tiny tech enhances healthcare, keep exploring the fascinating ways nanomedicine works inside your body.
Key Takeaways
- Nanomedicine uses nanoscale particles (1-100 nm) to improve diagnosis, treatment, and monitoring by navigating biological barriers effectively.
- Size, surface charge, and coatings like PEG influence nanoparticle circulation, targeting, and clearance in the bloodstream.
- Surface modifications with ligands enable precise targeting of specific cells or tissues, enhancing drug delivery efficiency.
- Stimuli-responsive systems release therapeutics on-demand, triggered by local pH, enzymes, or external stimuli like light or magnetic fields.
- Nanomedicine enhances treatment safety and efficacy by reducing side effects, improving bioavailability, and enabling personalized therapies.
What Is Nanomedicine and Why Is Size Important
Nanomedicine involves using nanoscale materials and devices—typically between 1 and 100 nanometers—to diagnose, treat, monitor, or repair biological systems. Your small size offers significant advantages: a high surface-to-volume ratio increases reactivity and interaction with biomolecules, enhancing effectiveness. Because of their size, these particles can navigate biological barriers more easily than larger agents. They also interact uniquely with proteins and cells, enabling precise targeting. The size influences how long nanomedicines stay in the bloodstream and where they accumulate. This control over biodistribution improves safety and efficiency. By tailoring the size and surface properties, you can optimize nanomedicine’s ability to reach specific tissues, deliver drugs effectively, and minimize side effects, making nanotechnology a powerful tool in modern medicine. Size-dependent properties are crucial for designing effective nanomedicines. Additionally, understanding the biological interactions at the nanoscale allows for the development of more sophisticated and targeted therapies, leveraging nanoscale interactions to improve therapeutic outcomes. Exploring nanomaterial design further enhances the potential for personalized and highly effective treatments.
How Nanoparticles Reach and Target Disease Sites
You can influence how nanoparticles travel through the bloodstream and reach disease sites by adjusting their surface properties and choosing appropriate targeting strategies. Surface modifications like PEGylation help them stay in circulation longer, while active targeting ligands direct them to specific cells. Triggering drug release with local signals such as pH or enzymes guarantees precise treatment at the intended site. Incorporating support breakfast concepts can also improve the biocompatibility and stability of nanoparticles within the circulatory system. Additionally, understanding the solar system helps inform the development of better energy-efficient technologies for medical devices. Recognizing the Youngster Choice can inspire innovative approaches to nanoparticle design and application. Exploring natural pools and their eco-friendly features can also inspire sustainable solutions in biomedical engineering. Moreover, applying principles of creative storytelling can enhance patient engagement and education regarding nanomedicine treatments.
Circulation and Distribution
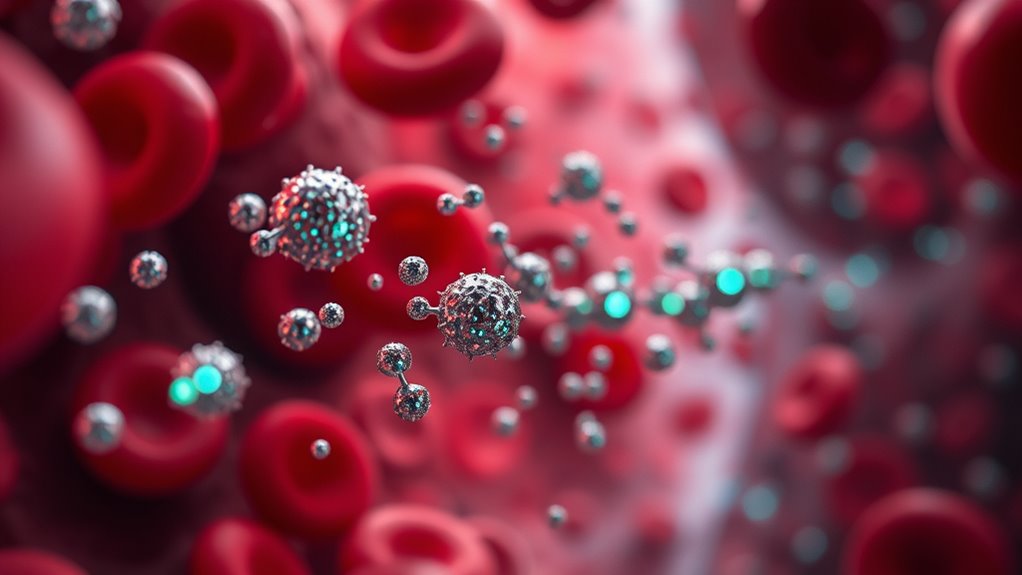
How do nanoparticles navigate the bloodstream to reach their intended targets? You play a key role in their journey, as size, surface charge, and the protein corona influence their path. Smaller particles (<8 nm) can be filtered by the kidneys, while larger ones (10–200 nm) avoid rapid renal clearance and stay in circulation longer. Surface modifications like PEG coating help evade immune detection, increasing half-life. Once in blood, nanoparticles circulate through vessels, influenced by blood flow and interactions with blood components. They may passively accumulate in tissues with leaky vasculature, like tumors, or be actively directed by ligands that bind specific cell receptors. Additionally, the size of nanoparticles determines their ability to penetrate tissue barriers, impacting their effectiveness in reaching disease sites. Furthermore, understanding the protein corona formation is crucial, as it affects nanoparticle behavior and targeting efficiency. Ultimately, their design determines how efficiently they reach and penetrate disease sites for effective therapy.
Surface Modification Strategies
Surface modification strategies are essential for guiding nanoparticles to their target sites and enhancing their therapeutic effectiveness. You can tweak nanoparticle surfaces with coatings like polyethylene glycol (PEG) to reduce immune detection and prolong circulation time. Attaching specific ligands, such as antibodies, peptides, or aptamers, helps the particles recognize and bind to disease-specific receptors, increasing targeting precision. Surface charge adjustments influence cellular interactions and biodistribution, with neutral or slightly negative charges often reducing nonspecific uptake. You may also incorporate stealth features to evade the immune system or add functional groups that respond to local environmental cues. These modifications optimize how nanoparticles navigate the bloodstream, avoid premature clearance, and arrive at the intended disease site effectively.
Targeting and Release Triggers
Nanoparticles are engineered to navigate the bloodstream and hone in on disease sites through sophisticated targeting strategies. Passive targeting exploits natural biological features, like increased permeability in tumors, to accumulate particles where needed. Active targeting involves attaching ligands such as antibodies or peptides that bind specifically to receptors on target cells, boosting uptake precision. To release drugs precisely, stimuli-responsive systems react to local triggers like pH changes, enzymes, redox conditions, light, or magnetic fields, activating payloads only at the disease site. These triggers enable controlled, on-demand therapy, minimizing side effects. Incorporating sustainable materials into nanoparticle design can further enhance biocompatibility and reduce environmental impact. Additionally, understanding targeting mechanisms is essential for optimizing nanomedicine delivery systems. Advances in drug delivery technologies are continually improving the accuracy and effectiveness of treatments. Integrating biocompatibility considerations helps ensure that these systems are safe for patients and the environment. Combining targeting with release triggers maximizes treatment efficiency, ensuring drugs act exactly where and when they’re needed most, and personalized approaches are increasingly being integrated to tailor therapies to individual patient profiles, further enhancing outcomes.
Types of Nanocarriers and Their Roles in Bloodstream

Among the various nanocarriers used in bloodstream applications, liposomes and lipid nanoparticles stand out for their ability to encapsulate both hydrophilic and hydrophobic drugs, enhancing solubility and protecting active agents from degradation. Liposomes are spherical vesicles with a phospholipid bilayer, ideal for delivering drugs that need to be released slowly or targeted specifically. Lipid nanoparticles, such as solid lipid or nanostructured lipid carriers, provide improved stability and controlled release. These carriers can be functionalized with targeting ligands or stealth coatings like PEG, extending circulation time and reducing immune detection. Their biocompatibility and versatility make them suitable for delivering a wide range of therapeutics, from cancer drugs to mRNA vaccines, ensuring efficient delivery while minimizing side effects.
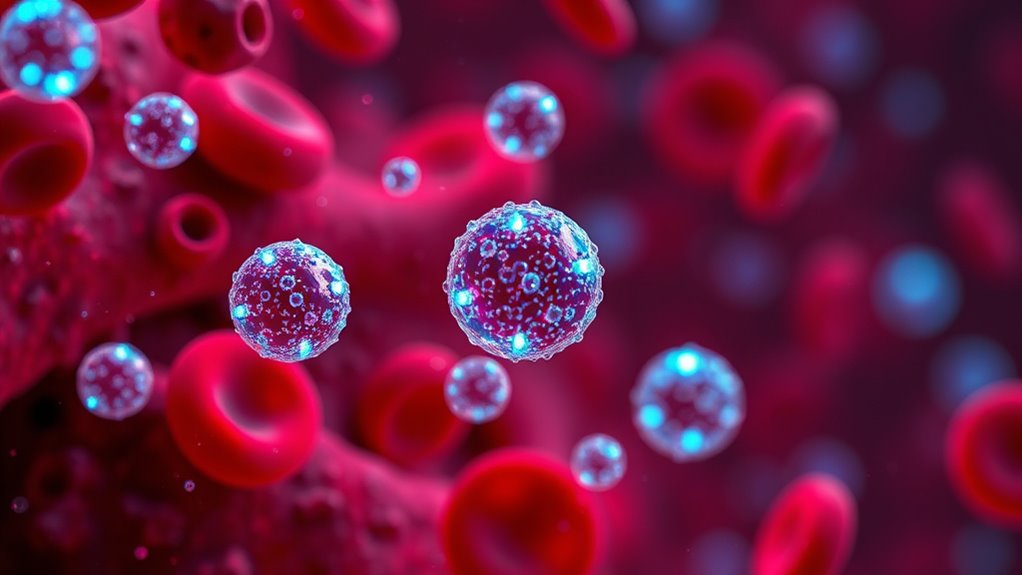
Once nanocarriers like liposomes and lipid nanoparticles enter the bloodstream, their journey through the body depends on a complex interplay of factors that determine where they go and how long they stay. You can influence their distribution by adjusting size, surface charge, and surface coatings like PEG, which help them evade immune detection and prolong circulation. The body clears these particles mainly through the kidneys, liver, or spleen, depending on their size and surface properties. Smaller particles (<8 nm) are filtered out by the kidneys, while larger or opsonized ones are captured by immune cells in the liver and spleen. Over time, protein adsorption, or the formation of a "protein corona," can accelerate clearance or alter biodistribution. Managing these factors helps optimize delivery and therapeutic efficacy.
Real-World Benefits and Success Stories in Clinical Settings

You can see how nanomedicine has transformed patient care through real-world examples that boost treatment effectiveness and minimize side effects. Approved nanomedicines like liposomal doxorubicin and mRNA vaccines demonstrate clear benefits, improving safety and expanding therapeutic options. These successes highlight how tiny tech is already making a significant difference in clinical outcomes. Additionally, ongoing innovations in nanotechnology applications continue to inspire advancements in nanotechnology research and application. Understanding affiliate relationships increasingly leverage nanotechnology to enhance diagnostics and targeted therapies, further demonstrating the transformative potential of this tiny tech in healthcare.
Enhanced Treatment Efficacy
Nanomedicine has revolutionized treatment outcomes by enabling highly targeted therapies that maximize efficacy while minimizing side effects. You see this in clinical successes like liposomal doxorubicin, which delivers chemotherapy directly to cancer cells, improving response rates and reducing toxicity. In infectious disease, lipid nanoparticles in mRNA vaccines have dramatically increased immune responses, leading to rapid, effective protection. For rare genetic disorders, nanocarriers enhance the bioavailability of poorly soluble drugs, making treatments more potent. Magnetic nanoparticles guide therapies precisely to disease sites, boosting effectiveness. These innovations result in higher success rates, lower doses, and fewer adverse effects. High-quality materials ensuring longevity and durability are also a key component of successful nanomedicine applications. Additionally, the development of targeted delivery systems allows for even greater precision in treatment, improving patient outcomes. Advances in nanoparticle manufacturing techniques have made these therapies more scalable and accessible to patients worldwide. The integration of biocompatibility considerations in design helps reduce immune responses and improve safety profiles. As a result, patients experience quicker recoveries, improved quality of life, and better overall outcomes, showcasing nanomedicine’s transformative potential across medical fields.
Reduced Side Effects
The targeted delivery capabilities of nanomedicine not only boost treatment success but also markedly reduce adverse effects. By directing drugs precisely to diseased cells, nanocarriers limit exposure to healthy tissues, decreasing toxicity and side effects. For example, liposomal formulations of chemotherapy drugs, like liposomal doxorubicin, deliver medicine directly to tumors, reducing cardiotoxicity and other systemic issues. Similarly, nanoparticles used in imaging minimize radiation doses while providing clearer diagnostics. These advances have led to fewer adverse reactions, improved patient comfort, and better overall outcomes. Clinical success stories highlight how nanomedicine’s precision helps avoid the collateral damage typical of traditional treatments, making therapies safer, more tolerable, and effective for a broader range of patients.
Approved Nanomedicine Examples
Have recent clinical advances truly demonstrated the tangible benefits of nanomedicine? Absolutely. Liposomal doxorubicin, approved for cancer treatment, offers targeted delivery that reduces side effects and enhances efficacy compared to traditional chemotherapy. Lipid nanoparticle mRNA vaccines—like those for COVID-19—show how nanocarriers enable rapid, effective immune responses with improved stability and safety profiles. Iron oxide nanoparticles are used in MRI to improve imaging clarity, aiding early diagnosis. Liposomal formulations of antifungals and chemotherapeutics increase solubility, bioavailability, and treatment precision. These examples prove nanomedicine’s potential to transform patient outcomes, offering more effective, safer therapies. As these innovations continue to advance, they pave the way for ongoing breakthroughs in personalized medicine and disease management.
Ensuring Safety: Challenges and Toxicity Concerns

Ensuring the safety of nanomedicine in the bloodstream presents a complex set of challenges rooted in the unique physicochemical properties of nanoscale materials. These tiny particles can generate reactive oxygen species, trigger inflammation, or activate the complement system, leading to adverse reactions. Some nanocarriers might accumulate unexpectedly in organs like the liver, spleen, or brain, raising concerns about long-term toxicity. Immunogenic responses, such as pseudoallergies, can occur after injections, compromising tolerability. Regulatory hurdles further complicate safety assessments because of difficulties in characterizing particles’ size, surface chemistry, and corona formation. Additionally, non-biodegradable inorganic nanoparticles pose risks of chronic buildup, making it essential to develop standardized testing methods. Balancing innovation with thorough safety evaluation is vital to translate nanomedicine into reliable clinical solutions.
Designing Smarter Nanoparticles for Better Outcomes

To advance the safety and efficacy of nanomedicine, designing smarter nanoparticles becomes a vital focus. You can achieve this by functionalizing particle surfaces with ligands like antibodies or peptides that target specific cells, improving precision. Incorporating stimuli-responsive materials allows the particles to release drugs only when triggered by local conditions such as pH or enzymes, reducing side effects. Using stealth strategies like PEGylation helps nanoparticles evade immune detection and prolong circulation. Combining diagnostic agents with therapeutics creates multifunctional particles that enable real-time monitoring of treatment. Optimizing size, charge, and surface properties enhances biodistribution and minimizes off-target accumulation. By integrating these smart features, you improve therapeutic outcomes, lower toxicity risks, and advance personalized medicine in bloodstream applications.
The Future of Nanomedicine in Bloodstream Applications
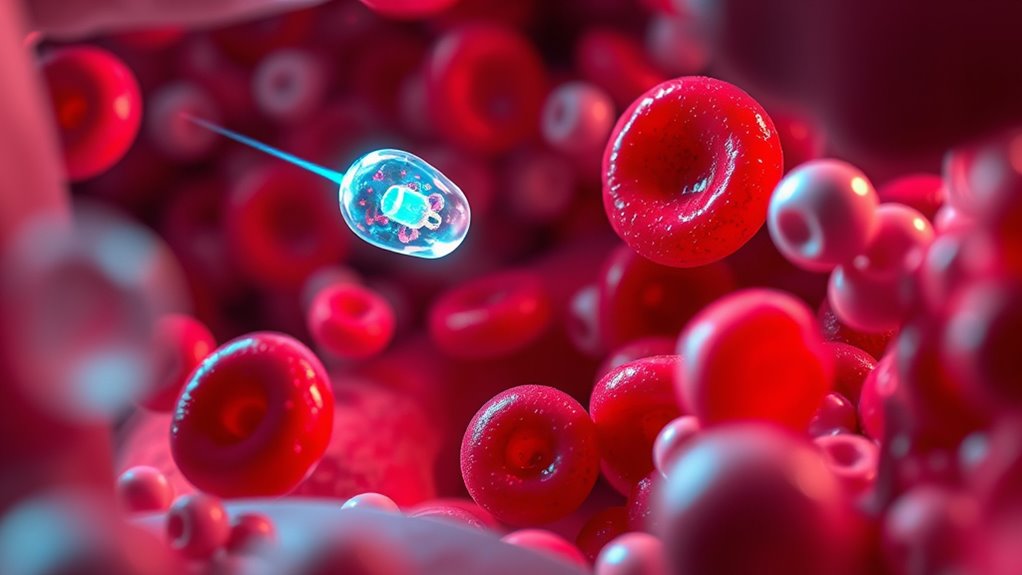
The future of nanomedicine in bloodstream applications is poised to transform personalized healthcare through the development of smarter, more responsive nanocarriers. You’ll see innovative designs that adapt to the body’s environment, releasing drugs only when needed. Advances in stimuli-responsive systems will allow precise control over drug activation, reducing side effects and increasing effectiveness. You’ll also benefit from multifunctional particles that combine diagnosis and therapy, enabling real-time monitoring of treatment progress. Targeting strategies will become more refined, using ligands and biomimetic coatings to improve specificity and circulation time. As safety and regulatory hurdles are addressed, expect more nanomedicines to reach clinics, offering personalized, minimally invasive treatments. This evolution will make nanomedicine a cornerstone of future healthcare, improving outcomes and quality of life.
Frequently Asked Questions
How Do Nanomedicines Avoid Immune System Detection in Blood?
You can avoid immune detection by nanomedicines through surface modifications like PEGylation or cloaking with cell membranes, which create a stealth layer that reduces opsonization. These strategies help the particles evade immune recognition, prolonging circulation time. Additionally, functionalizing their surfaces with specific ligands or coatings minimizes unintended immune responses, allowing nanomedicines to circulate longer and reach their targets more effectively.
What Are the Long-Term Effects of Inorganic Nanomaterials in the Body?
Long-term effects of inorganic nanomaterials in your body are like a shadow looming on the horizon. They can accumulate in organs like the liver, spleen, or brain, potentially causing chronic toxicity, inflammation, or oxidative stress over time. Some particles may persist due to limited biodegradability, raising concerns about long-term safety. Monitoring and understanding these impacts are vital to guarantee nanomedicine’s benefits outweigh possible risks in your health journey.
How Is Batch-To-Batch Reproducibility Achieved in Nanoparticle Manufacturing?
You achieve batch-to-batch reproducibility by standardizing manufacturing protocols, controlling raw material quality, and precisely regulating process parameters like temperature, pH, and reaction time. You also implement rigorous quality control measures, including size, surface chemistry, and purity assessments, using advanced characterization tools. Consistent documentation and validation make certain each batch meets strict specifications, reducing variability and ensuring reliable, reproducible nanoparticle production essential for clinical and regulatory success.
Can Nanomedicine Treatments Be Personalized for Individual Patients?
Yes, nanomedicine treatments can be personalized for individual patients. You can tailor nanoparticle designs by adjusting surface functionalization with specific ligands, targeting unique biomarkers, or modifying release triggers based on a patient’s genetics or disease profile. This customization enhances targeting accuracy, reduces side effects, and improves therapeutic outcomes. Ongoing advancements in diagnostics and biomarker identification support the development of personalized nanomedicines, making treatments more effective for each person’s unique biological makeup.
What Regulatory Hurdles Must Be Overcome Before Widespread Clinical Use?
You need to address regulatory hurdles like establishing standardized characterization methods for size, surface chemistry, and corona formation. You’ll also have to demonstrate consistent manufacturing processes, batch reproducibility, and safety profiles, including toxicity and immunogenicity assessments. Ensuring long-term safety, environmental impact, and clear guidelines for approval are essential. Overcoming these challenges requires collaboration with regulators to develop extensive testing standards, enabling nanomedicine’s safe and effective widespread clinical use.
Conclusion
Think of nanomedicine as a tiny ship steering your bloodstream’s vast ocean. With precise navigation and clever design, it reaches hidden islands of illness, delivering life-saving cargo. As you embrace this groundbreaking voyage, remember each nanoparticle is a brave explorer working tirelessly for your health. Together, they’re forging a new horizon—where health and hope sail hand in hand—turning science into a powerful beacon of tomorrow’s cures.